Joint Pain Treatment: Effective Solutions for Relief and Long-Term Recovery
Joint pain can really creep up on a lot of us. One day, you don't even think twice about it, and the next day, your knee or shoulder is being particularly cranky and slowing you down. Whether you have long-term and chronic arthritis, a recent flare-up from an old sports injury, or just creaky joints because you are getting older, the objective is the same: to find joint pain relief that is reliable and provides something for today, while also supporting long-term healing.
I have worked with individuals and groups across the life span and levels of physical activity, and one thing I have seen over and over again is, the best outcomes happen when people combine their good self-care choices with targeted professional treatments. There is no one miracle fix for everything. However, the right combination of exercise, nutrition, some simple home solutions, and medical interventions as needed, will support our goal of reducing pain and getting back to things we enjoy.
How Joint Pain Happens: A Simple Look
First, let’s clear up the main reasons joints hurt. Understanding the cause helps you choose the right joint pain treatment.
- Wear and tear. Osteoarthritis is the classic example. Cartilage thins, joint surfaces change, and movement gets painful.
- Inflammation. Conditions like rheumatoid arthritis involve the immune system attacking the joint lining. That creates swelling and ongoing pain.
- Injury. Ligament sprains, cartilage tears, and fractures can leave a joint unstable or painful long after the initial event.
- Crystal buildup. Gout and pseudogout cause intense flare ups when crystals form in the joint.
- Overuse and biomechanics. Weak hips, tight calves, or poor posture put extra stress on certain joints and lead to pain over time.
Each of these has distinct treatment priorities, for example while reducing inflammation will be central for rheumatoid arthritis, rebuilding strength alongside joint mechanics will be more important for overuse injuries.
When to See a Professional
Not every ache needs a doctor right away, but some signs mean you should get checked. Book an appointment if you have:
- Severe pain that started suddenly
- Swelling, redness, or fever with joint pain
- Failure to improve after a few weeks of self-care
- Joint locking, instability, or trouble bearing weight
- Known autoimmune disease or history of gout
In my experience, early evaluation can help prevent a small issue from becoming chronic. A clinician can order images and/or lab tests and provide a safer, quicker pathway to recovery.
Short-Term Joint Pain Relief: Practical Options You Can Try Now
You're probably looking for immediate relief. Here are widely used, evidence-backed methods to ease pain in the short term.
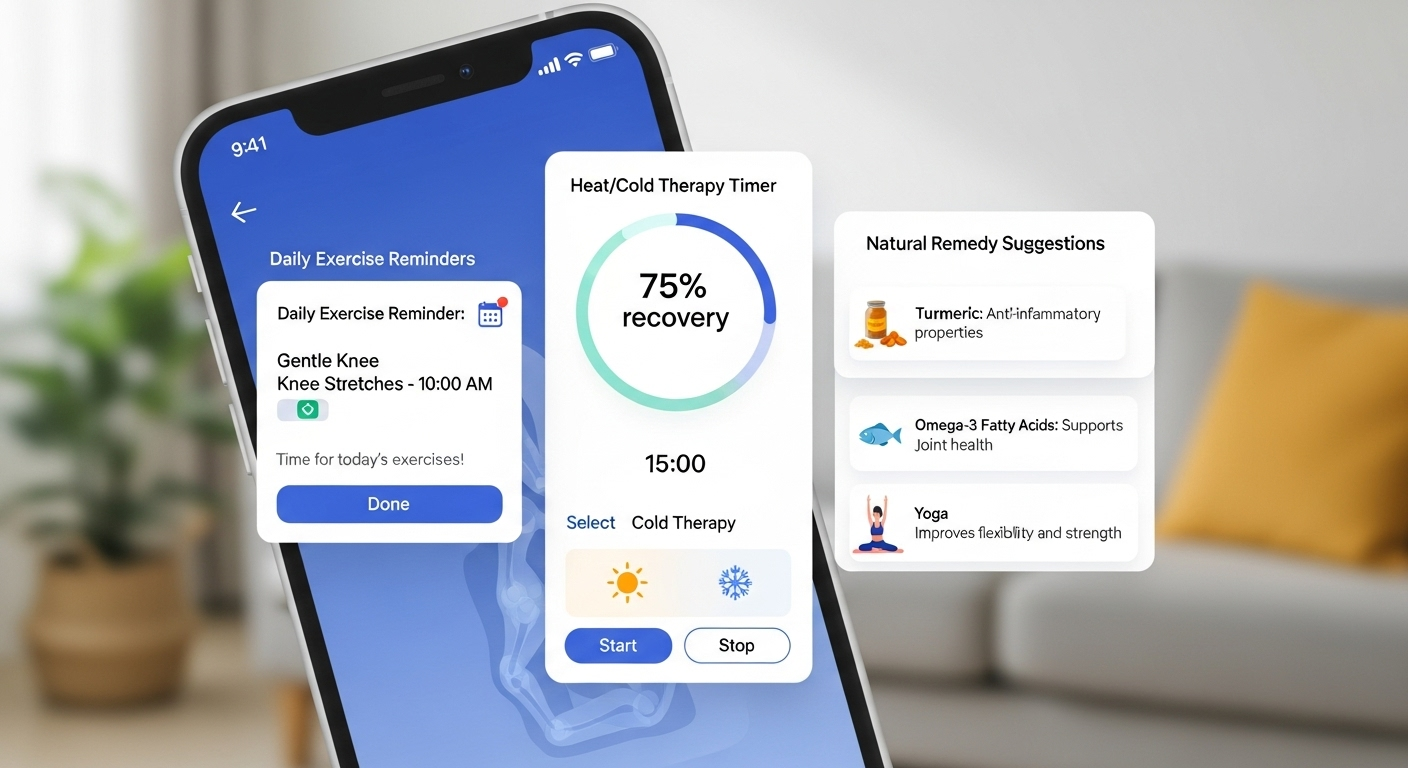
- RICE-ish method. Rest briefly when the pain is sharp then return to mild activity or movement. After again moving gently, ice to settle down swelling and numb pain. Heat is best for stiff and tight muscles to relax them.
- Over-the-counter medications. Nonsteroidal anti-inflammatory medications (NSAIDs) such as ibuprofen or naproxen can help manage inflammation and pain and fluids can provide some management for pain alone. Follow the dosing instructions and discuss any possible contraindications with your clinician.
- Topical medications. Gels, creams, and patches with NSAIDs or capsaicin or menthol can be effective in providing locally without exposure to systemic side effects.
- Compression and braces. A knee sleeve or wrist brace can improve function by minimizing the painful arc of motion and offer a sense of security during activity.
- Activity modification. Substitute high impact activities while the pain calms down with low impact alternatives, such as swimming or cycling.
These methods won’t fix the underlying problem in many cases, but they get you moving safely while you work on long-term recovery.
Natural Joint Pain Solutions That Actually Help
People ask me all the time: what natural remedies are worth trying? A lot of options exist, but some have better evidence than others. Below I share what I’ve found helpful with patients and clients.
- Omega-3 fatty acids. Fish oil reduces inflammation in rheumatoid arthritis and may ease joint pain in general. I tell people to aim for dietary sources first, then consider supplements after talking with a clinician.
- Turmeric and curcumin. These can reduce joint pain and inflammation for some people. The active compound needs proper formulation for absorption, so look for a reputable product.
- Glucosamine and chondroitin. Mixed results in studies, but some folks with osteoarthritis report less pain and better function. Try them for a few months and monitor changes.
- Collagen. Supplemental collagen peptides may help tendons and joint tissues over time when combined with exercise.
- Maintaining a healthy weight. This is one of the most effective natural strategies. Losing even a small amount of weight reduces joint load and pain in knee and hip arthritis.
A quick aside: natural does not mean harmless. Supplements can interact with medications and vary in quality. I always recommend checking with your healthcare provider and choosing brands that third parties test for purity.
Exercise and Joint Pain: Move to Improve
Movement is likely the most important long-term treatment for recovering from joint pain. I know that sounds obvious, but many people choose not to move, because it hurts. That’s the wrong choice. When done correctly, specific exercise can decrease pain, increase tolerance, and prevent future injury to the joint.
Here’s a practical approach that works for most joints.
- Begin by assisting with range of motion. Joint circles in a gentle manner, heel slides, and shoulder pendulum exercises can keep the joint mobile without a heavy loading.
- Proceed to strength training. Target muscles that support the joint. For example, an involved knee means involved quads, hamstrings, and hips. That strength will build on stability while putting less stress on the cartilage.
- Use low impact cardio too! Swimming, cycling, and walking can help get your blood flowing, as well as help the process of weight management.
- Create a safe environment for balance and proprioception. Using single leg stands, wobble boards, and gentle plyometrics can be helpful in preventing falls and re-injury.
- Finally, take your time in increasing load and intensity every other week or so. A sudden increase in activity is associated with setbacks.
Consider a structured program of eight to twelve weeks for measurable improvements. The great thing about physical therapists is that they will provide individualization and correct your technique, if you give any indication you are unsure. I have helped several clients recover from kneecap pain faster than expected simply by addressing a hip weakness that nobody thought mattered.
Physical Therapy and Manual Treatments
Hands-on therapy and guided exercise matter. A skilled physical therapist evaluates movement patterns, finds the weak links, and gives hands-on care to reduce pain.
- Manual therapy. Joint mobilizations, soft tissue work, and dry needling can reduce pain and make exercise easier.
- Exercise progression. Therapists tailor load, intensity, and specific exercises to your lifestyle and goals.
- Education. You learn joint-sparing movement patterns and how to manage flare ups at home.
I recommend physical therapy early after an injury and for chronic pain that limits daily activities. It’s often more cost effective long term than repeated imaging or temporary fixes.
Advanced Medical Treatments
Sometimes conservative care is not enough. Here are medical options that clinicians use for joint pain treatment. These require a doctor’s guidance and carry varying risks and benefits.
- Corticosteroid injections. These provide powerful short-term relief by reducing inflammation inside the joint. The effect can last weeks to months.
- Hyaluronic acid injections. Often used for knee osteoarthritis, these injections aim to restore joint lubrication and reduce friction.
- Platelet rich plasma and regenerative injections. PRP uses your own blood components to encourage healing. Evidence is mixed but promising in some situations.
- Biologic therapies. For autoimmune conditions like rheumatoid arthritis, targeted biologic drugs reduce disease activity and protect joints.
- Surgery. When structural damage is severe, procedures like arthroscopy, joint realignment, or joint replacement may be the best path to restore function.
Ask about risks, expected recovery time, and alternatives. I always encourage getting a second opinion before major procedures.
Daily Habits That Support Joint Health
Small, consistent changes add up. Here are practical habits I tell people to try first.
- Footwear matters. Supportive shoes reduce abnormal forces on knees and hips. Replace worn shoes every 300 to 500 miles.
- Sleep and recovery. Poor sleep increases pain perception and slows healing. Aim for consistent sleep and treat sleep apnea if present.
- Anti-inflammatory eating patterns. Focus on whole foods, vegetables, fatty fish, nuts, and limited processed sugars. It’s not a magic cure, but it helps.
- Stay hydrated. Joints need fluid balance. It’s basic, but people underestimate the role of hydration in tissue health.
- Modify repetitive tasks. Use assistive tools if your job or hobbies repeatedly strain a joint. Small ergonomic tweaks prevent flare ups.
Long-Term Recovery: Building a Plan That Lasts
Short-term relief is nice. Long-term recovery changes how you live. I prefer plans that combine measurable goals, progressive exercises, and checkpoints with clinicians.
Here’s a simple framework to follow.
- Assess and prioritize. Identify which joint limits your life the most and what activities you want to get back to. That guides treatment choices.
- Stabilize acute pain. Use medication, injections, or bracing to make movement possible.
- Rebuild capacity. Progressive strength and conditioning help the joint tolerate higher loads. Track strength, range of motion, and pain levels weekly.
- Maintain gains. Once function improves, shift to maintenance workouts and periodic check-ins with a clinician.
- Prevent relapse. Keep an eye on training load, sleep, body weight, and ergonomics to avoid backsliding.
Consistency wins. I’ve seen people regress after a burst of improvement because they returned to old habits too quickly. Slow and steady protects gains.
Common Mistakes and Pitfalls
Learning from others’ mistakes saves time and pain. These are frequent missteps I encounter.
- Ignoring pain signals. Pushing through sharp joint pain often makes things worse.
- Relying on passive treatments only. Massage or injections help, but they rarely replace exercise and movement for long-term improvement.
- Skipping progressive loading. Strength must be rebuilt gradually. People either do too much too fast or nothing at all.
- Blind supplement use. Buying multiple joint supplements without tracking effects or talking to a clinician wastes money and could cause harm.
- Thinking surgery is the only option. Surgery can be necessary, but exhausting conservative measures first usually leads to better outcomes.
A quick tip: document your symptoms, what helps, and what makes pain worse. That record is surprisingly helpful for your clinician and keeps you honest about progress.
Joint Pain Exercises: Simple Routines to Try
Here are easy exercises you can start today. They focus on knee, hip, shoulder, and general joint health. Do each movement slowly and with control. If pain increases significantly, stop and consult a clinician.
Knee
- Straight leg raises: 10 to 15 reps, 2 sets
- Mini squats to a chair: 8 to 12 reps, 2 sets
- Side-lying hip abduction: 10 to 15 reps each side, 2 sets
Hip
- Bridge holds: 10 to 15 seconds, 8 reps
- Clamshells: 10 to 15 reps each side, 2 sets
- Standing hip extension with band: 10 to 12 reps each side, 2 sets
Shoulder
- Pendulum swings: 1 to 2 minutes
- External rotation with light band: 10 to 15 reps, 2 sets
- Scapular squeezes: 10 to 15 reps, 2 sets
General mobility
- Cat cow for spine mobility: 8 to 12 reps
- Thoracic rotation on all fours: 8 to 10 reps each side
- Ankle pumps and circles to support gait and balance
These are starter moves. Progress to weighted or more challenging variations as pain decreases and strength increases. I like to pair them with short walks or pool sessions for cardio.
Special Considerations for Seniors and Caregivers
Seniors often have multiple issues: arthritis, balance problems, and reduced muscle mass. Caregivers play a big role in helping with safe long-term recovery.
- Focus on functional tasks. Sit-to-stand practice, stair negotiation, and carrying light loads improve independence.
- Prioritize balance training to prevent falls. Small improvements here greatly reduce hospitalizations.
- Ensure nutrition supports healing. Adequate protein, vitamin D, and calcium help maintain muscle and bone with age.
- Coordinate with clinicians to manage medications and any adverse effects that worsen joint pain.
From my experience, gentle regular movement and simple strength training reduce pain and increase quality of life more than passive treatments alone.
Tips for Fitness Enthusiasts Recovering from Injury
If you train hard, being sidelined by joint pain is frustrating. You want a plan that helps you return stronger without repeat injury. Here’s how to approach it.
- Identify the faulty link. Weak hips, poor ankle mobility, or imbalance often lead to knee or lower back pain.
- Maintain conditioning. If you can’t run, try swimming or cycling. Keep cardiovascular fitness while you rehab the injured joint.
- Use periodization. Gradually reintroduce intensity and volume. Short cycles of progressive overload help you rebuild without flare ups.
- Track objective metrics. Use measures like single-leg hop distance, squat depth, or pain scores to guide progression.
A practical example: if your left knee gives out during deadlifts, test hip strength and single-leg stability. Often, fixing hip control solves the knee problem in weeks, not months.
Monitoring Progress: What to Track
Recovery feels subjective, but tracking makes it objective. I recommend a small daily log with these items:
- Pain level on a 0 to 10 scale
- Activities you did and duration
- Mobility notes such as range or stiffness
- Sleep quality and mood
- Any medication or supplement changes
Weekly trends are more informative than day-to-day fluctuations. If pain steadily improves alongside increases in strength and function, your plan is working.
Natural Remedies to Avoid or Use Carefully
People assume natural equals safe. It is not that simple. Here are common remedies that deserve caution.
- High-dose herbal anti-inflammatories. Herbs like willow bark or high-dose turmeric can interact with blood thinners.
- Unregulated supplements. Some products contain contaminants or mislabeled dosages. Choose third-party tested brands.
- Excessive topical heating creams. Students of mine have burned their skin using too much menthol or capsaicin in one area.
- DIY injections or therapies. Anything invasive should be done by a trained professional.
Talk to a clinician about supplements and always start new products one at a time to notice effects or side effects.
When Surgery Makes Sense
Surgery is often framed as a last resort, and for good reason. Many joint problems respond to conservative care. But sometimes surgery provides the best long-term outcome. Consider it when:
- Severe structural damage limits function despite rehab
- Chronic instability leads to repeated injuries
- Pain is uncontrolled and prevents basic daily activities
Joint replacement has excellent outcomes for many people with end-stage arthritis. Recovery includes focused rehab and realistic expectations about timelines and function. If you face surgery, ask about expected recovery steps and alternatives before deciding.
Combining Treatments: A Realistic Example Plan
Here is a practical recovery plan for someone with moderate knee osteoarthritis who wants to stay active.
- Start with 2 weeks of activity modification and topical NSAID for flare control.
- Begin physical therapy focusing on range, quad strengthening, and hip control three times a week for 8 weeks.
- Introduce low-impact cardio such as pool walking twice a week to preserve conditioning.
- Start omega-3 and consider turmeric with clinician approval for inflammation control.
- Re-assess after 12 weeks. If pain persists and limits activity, consult orthopedics about injections or further imaging.
I’ve used this staged approach with many people. It keeps you active, addresses mechanics, and reserves invasive options for persistent problems.
Practical Tools and Accessories Worth Trying
Small tools often make a big difference in daily life. Here are items I recommend to clients.
- Supportive shoes with good midsole cushioning
- Adjustable insoles to improve foot mechanics
- Simple knee sleeve or wrist brace for activity
- Foam roller and lacrosse ball for targeted soft tissue work
- Resistance bands for home strengthening
These are low cost and low risk. Use them as part of a broader plan, not as standalone fixes.
What the Research Says and How to Interpret It
Research on joint pain treatments is large and sometimes confusing. Here are two principles I follow when reading studies.
- Look at clinical outcomes, not just imaging changes. A scan that looks better is not useful if your pain and function do not improve.
- Watch for study quality and conflicts of interest. Industry-funded trials can be helpful but deserve scrutiny.
In practice, combine evidence, clinical judgment, and patient preferences. That triad usually produces the best results.
Final Thoughts: Small Changes, Big Results
Joint pain treatment is rarely a single action. It is a process. You’ll get better results if you combine sensible short-term relief with a long-term plan that includes exercise, nutrition, and proper medical care when needed.
I’ve noticed people who keep simple habits stay active much longer. A little strength training, consistent movement, and attention to sleep and weight often beat flashy treatments. Treat recovery like training. Build capacity, progress slowly, and measure what matters.
Helpful Links & Next Steps
If you want to explore tailored joint pain relief plans or learn more about available treatments, you don’t have to do it alone. Find the Right Relief Plan Today: https://sutracms.com
Want a practical next step? Start a two-week log of pain, activity, and sleep. Bring that to your clinician or therapist. It makes appointments more productive and helps build a plan that actually fits your life.
Frequently Asked Questions (FAQs)
Q1. What is the most effective joint pain treatment?
There’s no single “best” treatment. The most effective approach usually combines exercise, nutrition, home remedies, and medical treatments as needed. A tailored plan based on the cause of pain gives the best results.
Q2. Can joint pain be treated naturally at home?
Yes. Options like omega-3-rich foods, turmeric, collagen, weight management, and gentle exercise can help. However, it’s important to check with a healthcare professional before starting supplements or new remedies.
Q3. When should I see a doctor for joint pain?
See a doctor if you experience sudden severe pain, swelling, redness, fever, persistent pain for weeks, or joint instability. Early medical evaluation helps prevent chronic issues.
Q4. Do I always need surgery for joint pain?
No. Most joint pain improves with non-surgical treatments such as physical therapy, injections, and lifestyle changes. Surgery is usually considered only when conservative treatments fail or when there is severe joint damage.